The 7-1-7 Alliance analyzed 505 bottlenecks from 148 outbreaks in 18 partner countries in Africa, Southeast Asia and the Americas to identify global patterns in the barriers to outbreak detection, notification and response. The results show consistency among the top bottlenecks as well as disease-specific trends. This simple analysis provides an example of how countries can leverage their own 7-1-7 bottleneck data to inform investments, prioritization and accelerate performance improvement.
How the 148 outbreaks performed against the 7-1-7 target

Above: Percentage of the 148 outbreaks analyzed by the 7-1-7 Alliance that met each component of the 7-1-7 target

Above: Percentage of outbreaks analyzed that met each component of the 7-1-7 target, by disease type
Overall, approximately 28% of outbreaks met the full 7-1-7 target. While detection (62%) and notification (75%) met the 7-1-7 target more frequently, only 47% of outbreak events met the response target. This suggests that while many countries are making progress with early warning, surveillance and notification systems, significant gaps remain in mobilizing timely and effective outbreak responses.
Certain disease categories consistently showed greater delays, indicating systemic weaknesses in addressing particular types of outbreaks.
- Viral hemorrhagic fevers (VHFs) and respiratory diseases (including COVID-19) had the highest percentage of events meeting the full 7-1-7 target (42% and 38%, respectively), likely due to heightened global attention, investment, and preparedness efforts.
- Cholera, vaccine-preventable diseases (VPDs), and vector-borne diseases showed the lowest performance (21%, 18%, and 18%, respectively). These diseases faced unique bottlenecks, including logistics delays, human resource gaps, and lack of diagnostic commodities.
7-1-7 bottleneck analysis
The 7-1-7 target enables countries to measure and analyze their performance on individual outbreaks to see where the detection, notification and response systems can be improved and what is working well. By conducting effective bottleneck analyses across outbreaks, countries can identify patterns of common bottlenecks––and enablers––that can inform their national health security strategies. Learn more on synthesizing and using results for planning.
Global bottleneck insights

Above: Percentages of the outbreaks that identified each bottleneck category, shown by phase of the outbreak
45% of bottlenecks occurred during the early response phase
Across all 148 events, 505 bottlenecks were identified, with 227 happening in the early response phase of the outbreaks.
Some early response activities, such as deploying a team to investigate the cause of an outbreak or laboratory testing to confirm a pathogen, provide information needed to initiate other response activities, such as initiating risk communication or deploying countermeasures. This path dependency means that bottlenecks affecting the earliest actions can have a compounding effect, making it more difficult to achieve a timely and effective overall response.
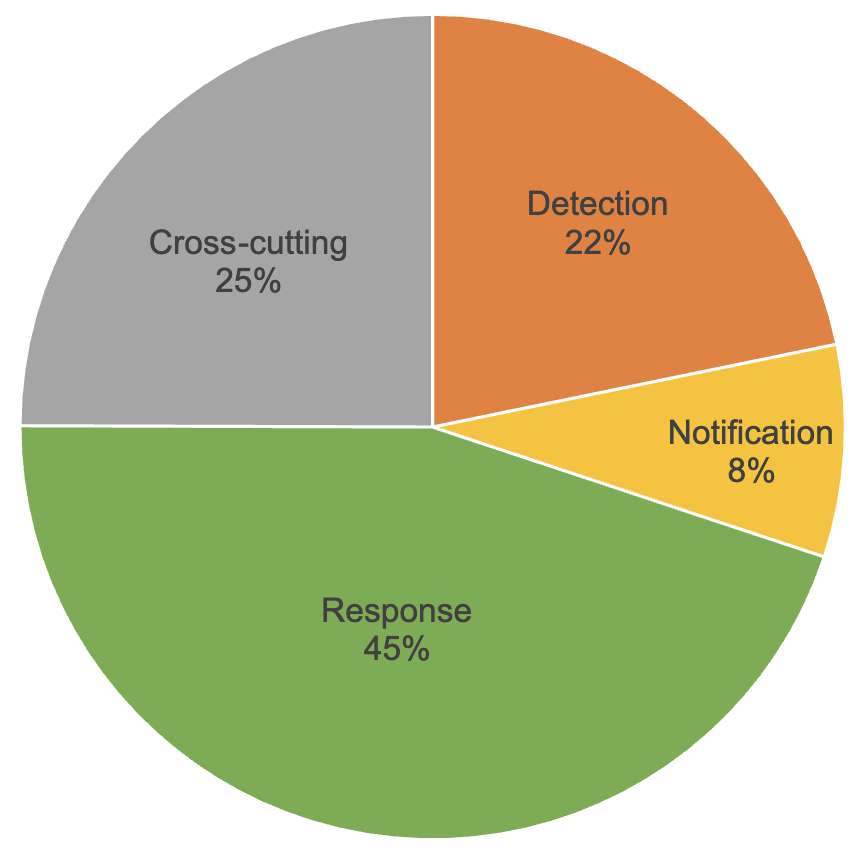
Above: Distribution of reported bottlenecks across outbreak detection, notification and response, and cross-cutting
Top 3 of the most common bottlenecks
The most common bottlenecks overall, which had the largest impact, were consistent across countries and outbreaks. They included:
Early response: Inadequate resource availability for 30% of outbreaks – See more insights
Detection: Low awareness or clinical suspicion for 28% of outbreaks – See more insights
- Early response: Laboratory confirmation for 27% of outbreaks – See more insights
Bottlenecks vary by disease type
Analysis of the most common bottlenecks highlights critical differences across disease categories in the underperforming disease categories [1]:
- Cholera outbreaks were seven times as likely to face logistics delays (four times as likely to report human resource shortages (14% vs. 3%), and nine times as likely to face a lack of diagnostic supplies (9% vs. 1%).
- Vector-borne disease outbreaks were twice as likely to experience competing priorities (10% vs. 4%) and access challenges (9% vs. 4%), and more likely to face delayed specimen transport (6% vs. 4%).
- Vaccine-preventable disease outbreaks were nearly twice as likely to report competing priorities (7% vs. 4%), and more likely to report failure of event verification (6% vs. 4%) and community knowledge and trust issues (5% vs. 3%).
These bottleneck differences by disease type may serve as a first step in understanding why health security systems achieve lower 7-1-7 target rates for outbreaks of these pathogens relative to other outbreaks. A full bottleneck analysis and deep dive of these trends in countries can further highlight the constraints that drive these lower 7‑1‑7 target rates.
[1] Percentages refer to the per cent of events of the reference disease type that reported that bottleneck compared to the per cent of all other events reporting that bottleneck (e.g., cholera vs. all non-cholera events).
How we categorized bottlenecks to identify patterns
We have developed a bottleneck taxonomy – a structured classification of common barriers to timely detection, notification, and response—based on analyses across several countries. The taxonomy facilitates cross-disease and cross-country analyses and pattern recognition and can be used to leverage 7-1-7 bottleneck data at the country level to inform the prioritization of investments.
How countries can leverage their own 7-1-7 bottleneck analysis to prioritize health security investments
Apply 7-1-7 routinely to highlight systemic constraints
Country implementation has demonstrated that 7-1-7’s bottleneck analysis approach is a useful tool for identifying systemic bottlenecks and corrective actions. Regular and routine application of the target for all outbreaks amplifies the evidence around system gaps and creates opportunities for further analysis to improve countries’ understanding of their performance.
Use bottleneck taxonomies to drive decision-making
A standardized approach to bottleneck classification can help countries and their partners identify systemic weaknesses and strategically allocate resources, even across multiple event types or implementing jurisdictions.
What we recommend:
- Establish routine bottleneck tracking as part of 7-1-7 outbreak assessments.
- Use taxonomies to identify patterns across event types, across implementing jurisdictions, and over time to prioritize interventions. We recommend using the 7-1-7 list of bottleneck categories as a starting point and adding additional bottleneck categories as needed.
- Use the bottleneck data – both single- and multi-event data – to identify short- and longer-term interventions to improve the performance of outbreak detection, notification and response systems; and to advocate for policies, budgets and investments to sustainably implement those interventions.
Share what you’re learning
Countries and their partners can collaborate through the 7‑1‑7 Alliance to exchange best practices in identifying, prioritizing and overcoming bottlenecks using 7‑1‑7.
What we recommend:
- Actively engage with the 7-1-7 Global Community of Practice (COP).
- Share case studies with the 7‑1‑7 Alliance to include in our COP case study repository accessible to all members.
- Consider peer learning exchanges with other COP countries that have similar outbreak challenges.
- Share 7-1-7 assessment findings and insights regularly with the 7‑1‑7
Alliance to create multi-country synthesis. Multi-country analyses can help identify certain programs, infectious diseases, or parts of the health security system which consistently under-perform (or perform effectively). They can yield additional insights on health security performance patterns which may exist independently from country-specific conditions (e.g., global program design, global health financing).