Previous posts in this series examined bottleneck trends across 500 bottlenecks from 148 outbreaks in 18 partner countries and explored solutions to resource barriers in outbreak response.
In this post, we dive into low clinical suspicion––the most common detection bottleneck––and promising initiatives that make a difference.
Low clinical suspicion can delay the full detection and response sequence
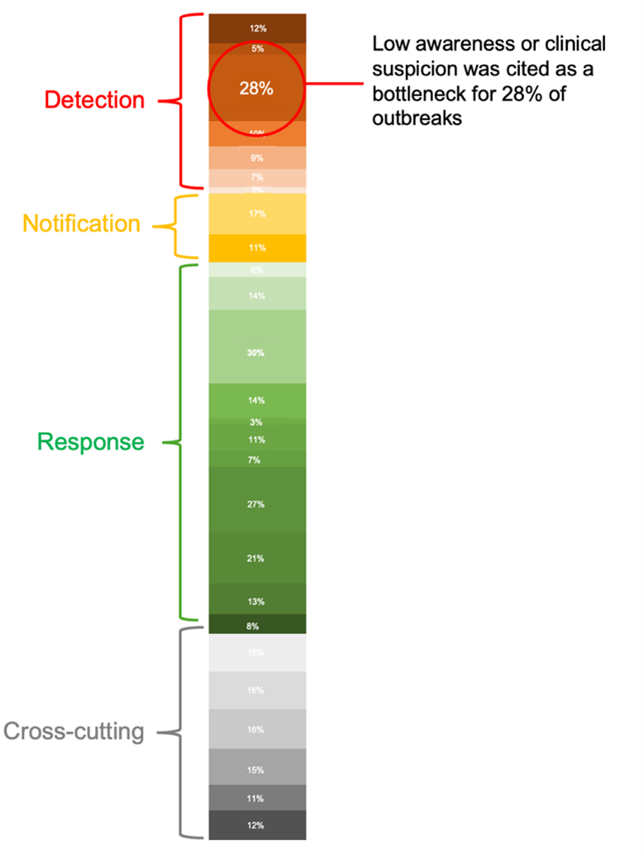
Above: Bottleneck synthesis showing how the 500 bottlenecks are distributed across 26 categories and four outbreak phases – see the full bottleneck synthesis in our previous post
A health care worker correctly detecting and immediately reporting new cases of infectious disease can mean the difference between an outbreak that is quickly contained and one that spirals into an epidemic.
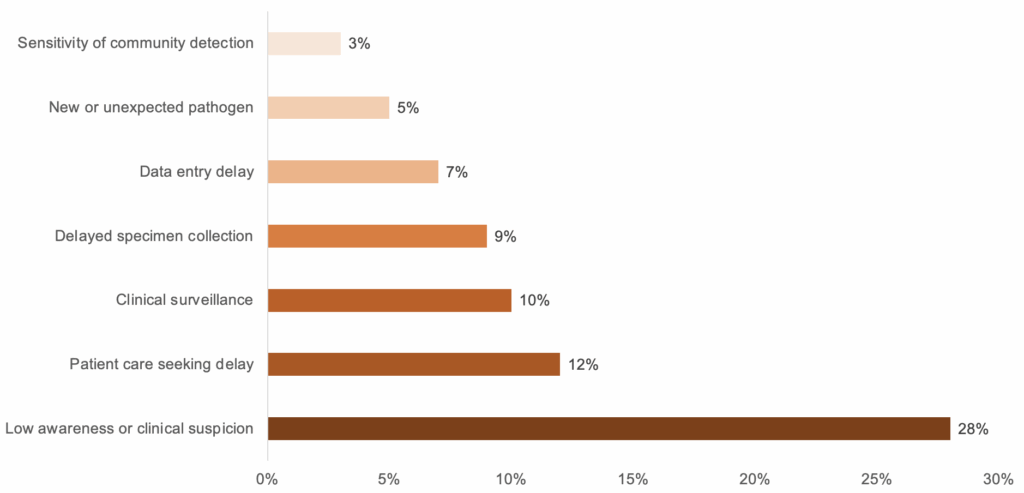
In our analysis, low clinical suspicion—health care workers failing to suspect an outbreak of disease—was the most common bottleneck to detection, cited in nearly one in three outbreaks (28%).
Low clinical suspicion is common, not only due to limited resources for training large numbers of frontline health workers in outbreak symptom recognition, but also because of gaps in continued medical education, standard operating procedures, confidence, and experience.
Identifying and addressing low clinical suspicion can be the biggest enabler of timely detection––and a gamechanger for response times.
Below: Frequency of detection bottlenecks. Low awareness or clinical suspicion was more than twice as likely to occur as the next most common detection delay.
Using 7-1-7 at the primary health care level
The majority of low clinical suspicion bottlenecks occur at the primary health care level. Primary health care is the frontline of epidemic detection but also plays a critical role in the response.
In 7-1-7, primary health care facilities typically contribute to meeting the 7-day detection and 1-day notification targets and one of the seven early response actions [1] (case management and infection prevention and control).
To better measure health facility readiness, Resolve to Save Lives (RTSL) has adapted the 7-1-7 target by focusing on three critical areas:
- Speed: How quickly cases are detected and notified, capturing the facility’s contribution to the seven-day detection and one-day notification targets of 7-1-7.
- Safety: How the facility immediately responds to ensure patient and health care worker safety, capturing the facility’s completion of three safety actions (isolation, treatment and personal protective equipment).
- Surge: How prepared the facility is to handle a potential increase in cases, capturing the facility’s completion of 10 critical “surge actions”[2] within seven days.
What solutions exist
An RTSL project supporting epidemic-ready primary health care (ERPHC) shows strong potential to improve clinical suspicion through simple, scalable interventions.
1. Mentoring health workers
Through the ERPHC initiative, RTSL is partnering with primary health care facilities to ensure they are epidemic-ready—able to prevent, detect, and respond to outbreaks within the 7-1-7 target while maintaining essential health services.
Each health facility in the program is receiving mentorship services for all its health care workers to elevate their knowledge, skills and confidence so they can spot symptoms, report suspected cases and keep themselves and their patients safe. Once a mentor is assigned to a facility, they develop an ongoing relationship with the workers, visiting them monthly. Mentors provide training and guidance, ensuring improved knowledge translates to improved detection, increased reporting and use of data to inform local practice.
The program was piloted in 703 partner health facilities in four countries.
Throughout its implementation, 31 ERPHC health facilities recorded a total of 207 confirmed cases of priority pathogens, such as mpox and yellow fever.
- 90% of cases met the seven-day detection target
- 100% of cases met the one-day notification target
- Only 26% of health facilities met all 10 surge actions, with the most common bottlenecks being inadequate supplies to manage further cases and limitations in physical infrastructure for isolation.
Ugandan districts increased alerts with ERPHC
In Uganda, ERPHC was implemented in 19 districts. Following implementation, these districts accounted for 57% of the country’s alerts—despite representing only 14% of all districts. They also generated fewer false alarms, indicating stronger clinical suspicion and improved detection capacity among health care workers.
2. Mobile training: Clinical Integrated Disease Surveillance and Response
Traditional face-to-face training for large numbers of health workers is expensive, complex, and creates staffing gaps in routine service delivery. Additional challenges include staff turnover, role changes, and the ongoing need for refresher training and onboarding of new employees. Innovative, cost-effective approaches that minimize work disruptions, are scalable to meet the needs of thousands of health workers and can be sustained over time, are essential.
RTSL collaborated with HealthLearn and frontline clinicians to design and implement Clinical Integrated Disease Surveillance and Response (cIDSR), a mobile phone-based training package specifically tailored for health care workers to improve their clinical suspicion to identify potential cases of epidemic prone diseases and improve their ability to immediately notify and care for patients.
cIDSR goes beyond case definitions for detection to reflect real patient presentations and the clinical reasoning that links symptoms to a possible case definition and the actions workers need to take to keep themselves and the community safe.
By designing the learning on mobile phones, cIDSR can scale to thousands of health workers in days instead of weeks, while still achieving improvements in knowledge.
In Nigeria, where clDSR was deployed:
- 12,000 health care workers enrolled in the course
- More than 60% completed the course, with an average 26% improvement in knowledge scores.
- 98% of workers said that the course provided them with a higher index of clinical suspicion for priority pathogens in patients presenting with an unknown illness.
In Uganda:
- Nearly 15,000 health care workers enrolled in cIDSR
- 69% completed the course and achieved similar 26% learning gains.
The deployment of cIDSR training is not just high impact; it’s also cost effective. Because it eliminates travel, accommodation, venue and facilitator expenses, online training like cIDSR can be more cost effective than traditional in-person training. The cost to develop the learning platform and course for one cIDSR module was $3 per health care worker compared to about $61 for the in-person equivalent according to an RTSL estimate.
Nigeria’s just-in-time cholera module
When Nigeria declared a cholera outbreak in June 2024, Resolve to Save Lives released a cholera response cIDSR module within 48 hours. In just three days, the training reached 3,000 health care workers, increasing to over 8,000 nationwide within five weeks; uptake targeted known cholera hotspots like Lagos thanks to the crucial support from the Nigeria Center for Disease Control. Among those who completed it, average knowledge scores increased by 29% from pre- to post-test, and more than 98% reported increased confidence in identifying and reporting suspected cholera cases.
Measuring impact: Testing clinical suspicion with patient simulations and real-world outbreaks
To confirm these promising results and further assess the impact of ERPHC on clinical suspicion, RTSL and partners coordinated 58 patient simulation exercises at facilities enrolled in the program. The exercises were designed to mimic real outbreak scenarios and test whether health care workers took appropriate actions to stop the outbreak and keep themselves safe.
The simulations provided additional insights into the real-world performance of health care facilities.
- Across the 58 exercises, 71% identified the correct diagnosis, which is a marker of clinical suspicion and related to detection.
- Health facilities performed equally well regardless of the priority pathogen used during the simulations.
- In Ethiopia, ERPHC facilities outperformed non-ERPHC facilities and were three times more likely to complete all necessary actions.
Another way to measure ERPHC’s impact was to apply the adapted 7-1-7 target (speed, safety, surge) to real-world outbreaks. In Sierra Leone, public health authorities applied the adapted target to 174 confirmed Mpox cases and compared performance between 12 ERPHC and 10 non-ERPHC facilities.
- The results showed that investments in ERPHC yield better performance during outbreaks across speed, safety, and surge.
- Notably, 83% of cases were detected within seven days at ERPHC facilities compared to 79% at non-ERPHC facilities. In addition, statistically significant differences were found for safety and surge.